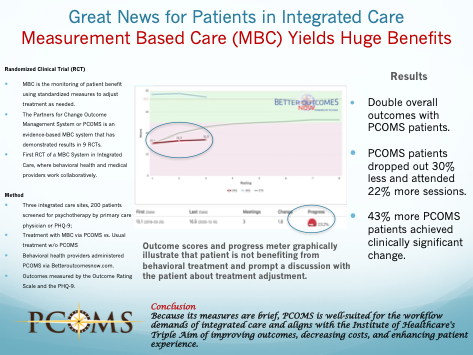
Huge Benefits for Patients in Integrated Healthcare Using PCOMS!
Great news for patients receiving treatment in integrated healthcare, where behavioral health and medical providers work collaboratively to address patient needs. The first study of measurement-based care (MBC), the monitoring of patient benefit using standardized measures to adjust treatment as needed, has demonstrated dramatically better results with patients reporting mental health concerns.
Using the Partners for Change Outcome Management System (PCOMS), a widely researched MBC intervention and its web application, Better Outcomes Now, PCOMS was evaluated in three integrated Federally Qualified Health Care Centers in Colorado. The study conducted by Drs. Barry Duncan, Jeff Reese, and colleagues, published in Families, Systems, & Health reported:
- Double overall outcomes with PCOMS patients.
- PCOMS patients dropped out 30% less and attended 22% more sessions.
- 43% more PCOMS patients achieved clinically significant change.
Because its measures are brief, PCOMS is well-suited for the workflow demands of integrated care and aligns with the Institute of Healthcare’s Triple Aim of improving outcomes, decreasing costs, and enhancing the patient experience.
Abstract
Introduction: Many suggest that the next step for integrated care is the widespread implementation of measurement-based care (MBC). While the measures most associated with MBC are standardized, no randomized clinical trial has demonstrated their use to improve psychotherapeutic outcomes with embedded behavioral health providers in integrated care.
Two evidence-based MBC systems have been studied in a variety of behavioral health environments but neither system has been investigated in an integrated healthcare setting. Addressing this gap in the literature, this study evaluated the use of MBC, specifically the Partners for Change Outcome Management System, in three integrated care sites.
Method: Using a randomized design within routine care, treatment as usual (TAU; n = 133) was compared using the Outcome Rating Scale (ORS) and Patient Health Questionnaire-9 (PHQ-9) with a feedback condition (n = 147) in which behavioral health providers had access to patient-generated outcome (ORS only) and alliance information at each session.
Results: Patients in the feedback condition demonstrated significantly more improvement than those in the TAU condition post-treatment on the ORS. Patients in the feedback condition also achieved significantly more clinically significant change as measured by both the ORS and PHQ-9. Feedback condition patients also attended significantly more sessions and dropped out significantly less than TAU patients.
Discussion: While preliminary and not without mixed results, this study offers evidence from the intervention measure (ORS) and the PHQ-9 that the documented improved outcomes and reduced dropouts associated with MBC in traditional behavioral health centers may also occur in integrated care settings.
Reference
Duncan, B. L., Reese, R. J., Lengerich, A. J., DeSantis, B., Comeau, C. V., & Johnson-Esparza, Y. (2021). Measurement-based care in integrated health care: A randomized clinical trial. Families, Systems, & Health, 39(2), 259–268. https://doi.org/10.1037/fsh0000608
{{cta(‘cbe81f3e-7a7e-4c9f-8668-4fd6a37b51d0’)}}
